https://writeripple.com/etiology-of-renal-failure-causes-risks/Introduction: The role of breast ultrasound in cancer detection
We are always researching what percentage of breast ultrasounds are cancer and we do lot of analysis, studies and find information’s. Breast ultrasound plays a crucial role in the early detection and diagnosis breast cancer. As an imaging modality that does not involve radiation exposure, ultrasound is particularly well-suited for assessing breast lumps and distinguishing between solid masses and fluid-filled cysts. The major alternative imaging technique used for breast cancer detection, mammography, relies on X-rays to produce detailed images of breast tissue.
However, because X-ray images do not always create accurate pictures of dense breast tissue, a significant number of breast cancer cases are found only after an ultrasound examination, or the patient may be asked to undergo. It is not just a question of the accuracy of the ultrasound: despite its high sensitivity to breast lumps, it is very uncommon to diagnose cancer with the first ultrasonography.
Specifically, only 2-7% of cases present cancers as detected during the procedure – most patients with breast lumps have benign conditions, such as cysts or fibroadenomas. Nevertheless, ultrasound is a valuable modality precisely because it is rarely the only test performed – that is, it is complementary to other imaging techniques.
As such, the radiologist uses breast ultrasound results to understand whether further examination or biopsy is necessary. Ultimately, the majority of lumps detected using ultrasound for breast lumps are benign; however, breast ultrasound is used in most imaging cases to ensure timely and precise cancer diagnosis when necessary.
How does a breast ultrasound work?
A breast ultrasound is a non-invasive imaging test that utilizes high-frequency sound waves to produce comprehensive images of the internal breast structures. When a breast ultrasound is done, the technician rubs a gel on the skin and moves a small piece of equipment called a transducer over it. The transducer emits sound waves into the breast tissue; when the waves bounce back, the system converts them into real-time pictures on the screen.
Breast ultrasounds are successful in identifying abnormal growth, such as cysts and solid masses, as well as changes in the breast tissue that may not be visible in other imaging scans. Mammograms use a low-dose X-ray to create images, whereas ultrasounds, do not emit radiation and are commonly utilized as a supplementary instrument when mammogram results are inconclusive or while scanning dense breast tissue.
Mammography, MRI, and Ultrasound are the three types of breast imaging available today. Mammography detects calcification and cancers before other scanning types due to its high sensitivity. For high-risk individuals, MRI can obtain very clear photos. Ultrasound may further distinguish if a cyst is fluid-filled from solid.
The question one could ask is what percentage of breast ultrasounds are cancer? When women receive diagnostic breast ultrasound due to irregular screening, research shows that just 2-3% of patients detected to have cancer are diagnosed. Most results are cysts or fibroadenoma growths, both of which are benign. This illustrates how crucial it is not only to obtain good images with good information, but also to generate them efficiently.
Understanding Results: What are the Implications of a Breast Ultrasound Finding on the Health of Patients?
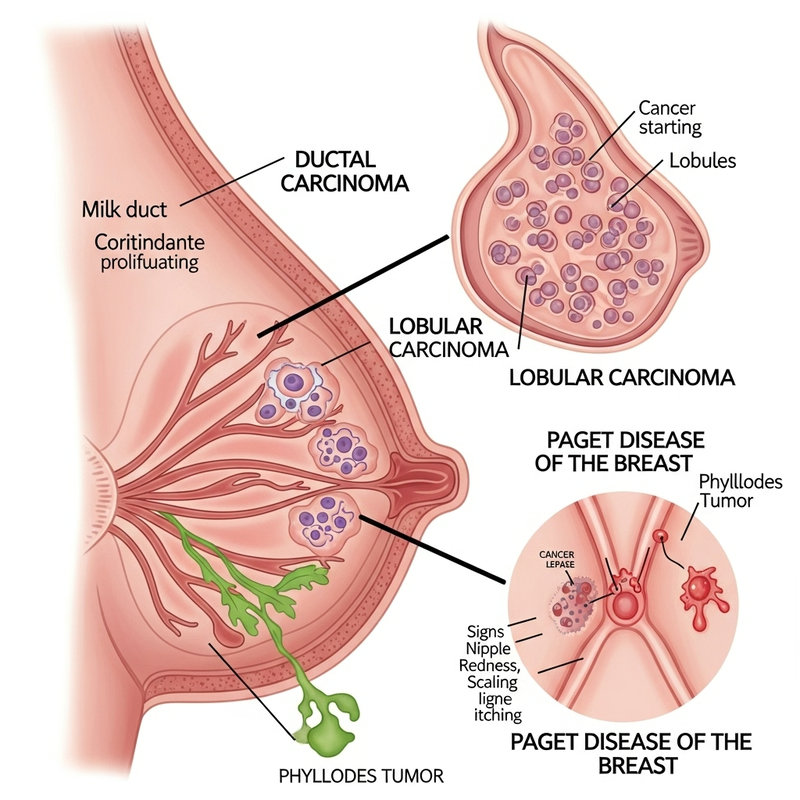
As much as breast ultrasounds have their fair share of vital diagnostic contribution, they are designed to differentiate observations as either benign or malignant conditions. Benign observations like cysts and fibroadenomas are very common among breast examinations, and they typically do not point towards any abnormal cause. Malignant observations like cysts and fibroadenomas can be detected at minimal levels.
However, typically, only 2-7% of ultrasound observations made are observed to be malignant. When the results from your ultrasound confirm an abnormality, your care provider may recommend further tests such as an MRI or a mammogram to ascertain the diagnosis. On the worst-case scenario, they may call for a biopsy. This situation does not imply that every observation from an ultrasound is always cancerous. Many cases do not require further practices as they can be observed over time or ignored if they pose no threat.
The results can therefore be very challenging to figure it out, but the aspect that most are non-cancerous should give one peace of mind. It may all work in vain if one does not seek further clarification from their medical teams. If further practice is recommended, they should be consulted, since that is their goal in a patient’s life.
The Key Statistic: What Percentage of Breast Ultrasounds are cancer?
The first and crucial piece of information is the breast ultrasound’s success rate in cancer detection, which interests both patients and health workers. The question is: “what percentage of breast ultrasounds are cancer”? Various studies have shown that on average 2 to 7% of breast ultrasounds performed due to suspicious findings indicated the cancer. Therefore, City of Hope emphasizes that the majority of abnormalities found due to breast ultrasound turns out to be benign.
The positive predictive value of breast ultrasound is influenced by the signs of the lesion and risk factors of the patient. For example, if an ultrasound shows a solid mass with irregular and other suspicious margins, the PPV is much higher in contrast to cystic or well-defined lesions. Another key point is to consider the frequency of diagnostic use: as far as mammography is still the primary approach to cancer detection, ultrasound frequently finds the cancer that was beyond the mammogram’s capabilities to show, which is possible since ultrasound is beneficial for women having dense breast tissue.
Patients have their risk of the disease too, contributing to both the possibility of malignancy and the prevalence of test results declaring one. Thus, while the substantial part of ultrasounds doesn’t display a malignant abnormality, this method is still quite beneficial for a comprehensive approach based on the individual assessment of risks.
How many factors influence the likelihood of a cancer diagnosis following breast ultrasound?
It’s critical to recognize that a number of critical elements influence both detection rates and results when determining the proportion what percentage of breast ultrasounds are cancer. One of the most important is the patient’s age and age. Naturally, young women have denser breast tissue, which complicates the process of interpreting both mammography and ultrasound examinations. Dense breast tissue is also a risk factor for cancer itself, as it makes it difficult for imaging tools to distinguish between suspect areas and benign tissue.
Another crucial factor is the patient’s family history. If a woman has close relatives who have been diagnosed with breast cancer, the likelihood of an abnormality that may warrant further monitoring or testing increases. The BI-RADS assessment categories also allows radiologists to talk about the degree of suspected cancer based on the ultrasound. The categories contain BI-RADS 1 to BI-RADS 5, with the second being entirely negative and the fifth highly suggesting malignancy and dictating a follow-up.
In conclusion, the most important thing to absorb is that most breast ultrasound findings are benign. Citing a variety of sources, the study notes that only somewhere between 2 and 10% of all suspect lesions will turn out to be cancer. Naturally, this proportion has many factors both patient-dependent and contingent based on the assessment radiologists make.
What Happens After an Abnormal Breast Ultrasound Result?
So, you’ve gotten an abnormal breast ultrasound result – now what? Although this news can be scary, remember that most suspicious abnormalities are not cancer. In fact, only about 20% of breast ultrasounds are cancer when a biopsy is performed. This means that the majority of suspicious results are revealed as benign.
The exact next steps after an ultrasound finding depend on the characteristics of the imaging finding. Common next steps include further imaging tests such as diagnostic mammography or MRI to gather more information and determine whether further steps are warranted. These imaging tests are used to determine if a lump or finding is a simple cyst, for example, or if it has other features that might make it concerning.
Additional imaging may also prove inconclusive or confirm that the finding is highly suspicious of cancer. In this case, your doctor is likely to recommend a biopsy. Minimally invasive biopsies remove just a small tissue sample from the concerning spot, which is then sent to the lab for analysis. Your doctor will advise you as to which type of biopsy is best for you. It may be a fine-needle aspiration or a core needle biopsy depending on the size and location of the concerning finding.
All in all, your medical team is there to guide you all along the way and assist you with any burning questions, including “what percentage of breast ultrasounds are cancer?” and “which is the least invasive follow-up method in my case?” In the end, quick follow-up leads to the rapidly necessary start of appropriate treatment if needed, gives you peace of mind if there is no cause for concern.
Breast Ultrasounds and Cancer Detection FAQs
- 1. What percentage of breast ultrasounds are cancer?
Generally, only 2–7% of breast ultrasounds performed for suspicious findings result in a cancer diagnosis.
- 2. Are most breast ultrasound findings cancerous?
No, the vast majority of breast ultrasound results are benign, such as cysts or fibroadenomas.
- 3. If an ultrasound finds a lump, is it likely cancer?
Most lumps detected by ultrasound turn out to be non-cancerous; only a small percentage are malignant.
- 4. How accurate is breast ultrasound for diagnosing cancer?
Breast ultrasound is highly sensitive for detecting lumps, but only a small percentage (about 2–7%) confirm cancer.
- 5. Can a benign result occur after a suspicious ultrasound?
Yes, even when a result appears suspicious, around 80% of biopsied findings are benign, not cancer.
- 6. Does everyone with an abnormal ultrasound need a biopsy?
Not always. Many abnormal findings end up being non-cancerous and simply require monitoring.
- 7. Why do so few breast ultrasound findings prove cancerous?
Ultrasound is designed to identify all irregularities, but most are benign conditions rather than cancer.
- 8. How does breast tissue density affect cancer detection in ultrasound?
Dense breast tissue can hide cancers on mammograms, making ultrasound useful, though only a minority of findings are cancer.
- 9. What factors increase the likelihood that an ultrasound finding is cancer?
Older age, a family history of breast cancer, and highly suspicious imaging features raise the chances, but percentages remain low overall.
- 10. Should I worry if my breast ultrasound finds something?
Most findings are not cancer—about 93–98% are benign—so follow-up is routine but not usually cause for alarm.
Conclusion: Know Your Risk and the Importance of Regular Screening.
Breast cancer is one type of cancer where the chances of patient survival increase dramatically with early detection. Regular testing can reveal possible abnormalities in the breast long before symptoms form. For those who wonder what percentage of breast ultrasounds are cancer: the vast majority of breast ultrasounds that are carried out result in a benign finding. Estimates suggest that between 2 and 4 percent of breast ultrasounds result in a diagnosis.
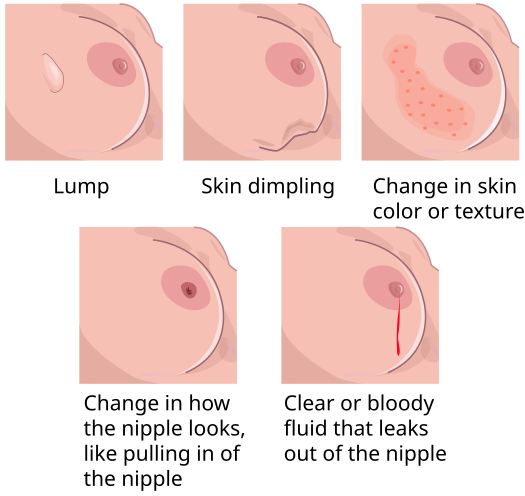
It is essential to know when to contact your primary care physician. As previously mentioned, whether there are lumps or nipple discharge or whenever breast pain becomes consistent, it is time to seek medical attention. Personal risk factors should be analyzed with your healthcare provider to determine the most appropriate screening schedule for your needs.
When both mammography and ultrasound are combined, the accuracy level increases, and incidents are detected early. By regularly monitoring your danger and testing yourself, you can take isolated measures to provide the ideal possible environment for maintaining health.